
How ZMA Can Boost Your Immune System
Wondering how to boost your immune defences and fight against illness? Discover the science of ZMA and how it can help your immune system.

How does the body produce testosterone?
How does it get distributed and used across the body?
What methods can be employed to leverage these mechanisms and ensure healthy testosterone levels?
These are questions most men have thought about at some point, but likely couldn’t get a clear answer to when searching the internet. This page answers these. It answers them in a way which can be easily understood, allowing any man to optimise their hormones and overall health.
By understanding how the testosterone system works, we can work to leverage it. In doing so, we can increase low testosterone levels and avoid testosterone deficiency. This approach enables the natural systems already in our bodies to regain their functionality, rather than bypassing them with unnatural treatments and testosterone replacement therapy.
After all, nature created these systems for a reason. We should use them to keep our health and longevity.
This flow chart visualises how testosterone is produced and distributed across the body in adult males. The following page explains this system in more detail. You should refer back to this graphic as needed to clarify explanations.

Testosterone production happens in the Hypothalamic-Pituitary-Gonadal (HPG) axis. This is the system of interactions between the Hypothalamus, Anterior Pituitary Gland, and Male Gonads (Testes). After it is produced, it is then distributed across the body through the blood.
Like most things that happen in our bodies, the testosterone production system begins in the brain. First, in the Hypothalamus, and second, in the Anterior Pituitary Gland. These systems regulate and control other systems in the body when functioning properly, and of importance to this page, contribute to maintaining normal testosterone levels.
The hypothalamus begins a series of hormone releases leading to testosterone production. It is a small part of the brain that acts like a control centre for many important functions in the body, including the regulation of body temperature, hunger and thirst, sleep cycles, and hormone production.
The hypothalamus determines when to produce testosterone based on signals from the testes in men and ovaries in women, the circadian rhythm, neural signals from other areas of the brain, and the blood levels of other hormones. It then releases Gonadotropin-Releasing Hormone (GnRH), sending it to the anterior pituitary gland.

The anterior pituitary gland is located at the base of the brain and releases several hormones that control different parts of your body. These include growth, reproduction, sex hormones, and thyroid function.
The gland acts as a messenger, telling other glands in the body what they need to do to keep the body functioning properly. Once it senses GnRH (sent from the hypothalamus), it releases Luteinizing Hormone (LH) into the blood.

The brain’s release of luteinizing hormone acts as a signal to produce testosterone in leydig cells.
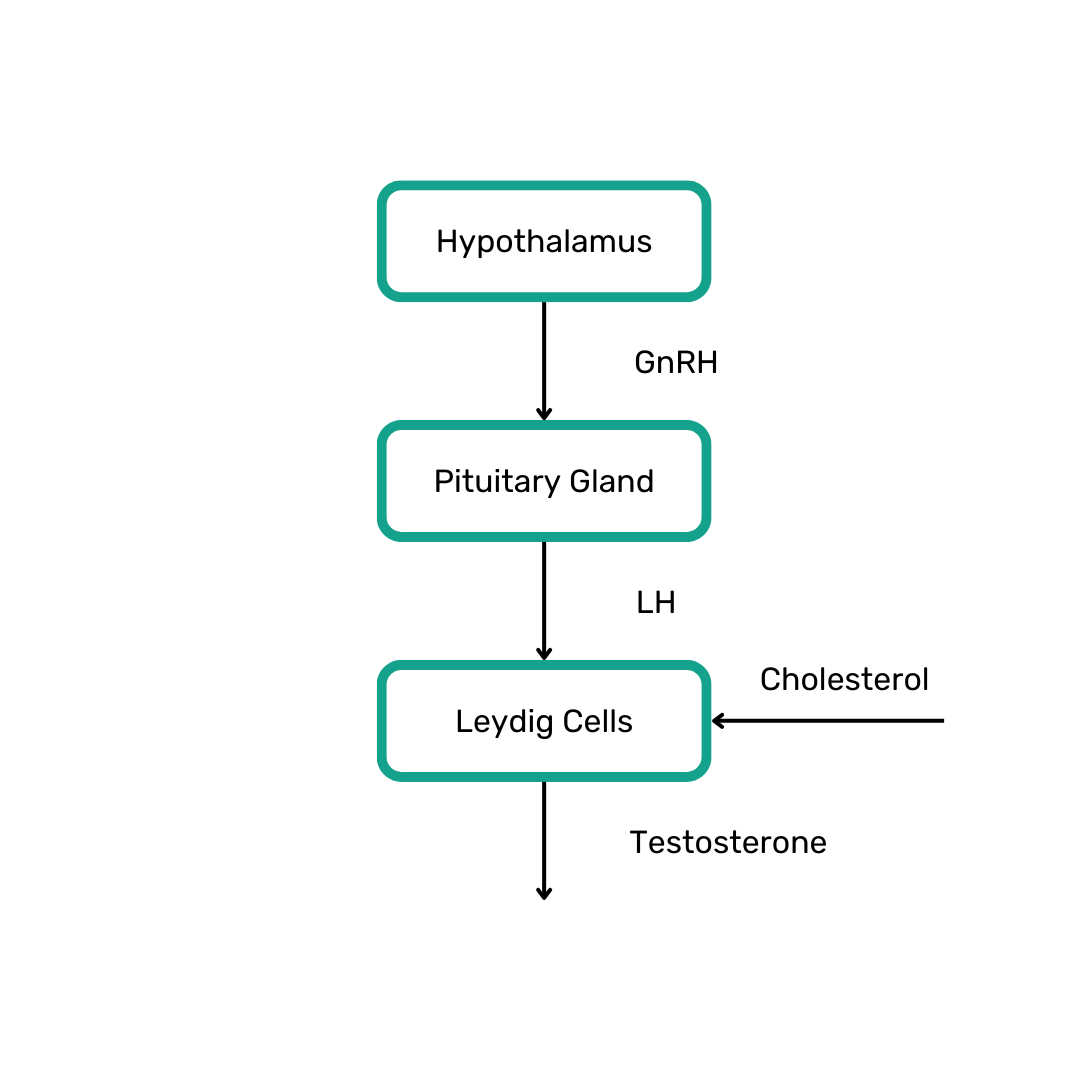
Within men’s testes, leydig cells are responsible for receiving the luteinizing hormone signal created by the anterior pituitary gland. They use the signal to initiate the production of the male sex hormone.
To do this, they take cholesterol and then converted it into testosterone, where it is then released into the blood.
Adrenal glands also produce a small amount of testosterone in both adult men and women. They do so as a result of the pituitary gland sending Adrenocorticotropic Hormone (ACTH) to them.
In men, the vast majority of testosterone is produced by leydig cells in the testes. As such, this page focuses on production from leydig cells, and how it can be optimised, rather than what is created by adrenal glands.
Once produced, circulating testosterone is transported by the blood to different areas of the body.
Once in the bloodstream, various processes utilise and transport it in different ways. The following section describes the different components that make up circulating testosterone and what it is converted into.

40-60% of testosterone produced binds to something in the blood called Sex Hormone-Binding Globulin (SBHG).
SHBG is a protein that the liver produces, which attaches to sex hormones in the bloodstream. Its primary role is to transport and regulate the distribution of sex hormones throughout the body by binding them after they are produced. In doing so, it makes testosterone less bioavailable, and therefore less effective.
The level of SHBG impacts the amount of free (unbound) circulating testosterone available for use in tissues and organs. Low levels of SHBG allow for higher levels of free testosterone, thereby making it more effective. High levels of SHBG do the opposite.
To maximise the efficacy of testosterone, SHBG should be minimised. By doing so, the quantity of free and active testosterone available for use across the body increases.
As men age, SHBG increases every steadily every year. So much so that free testosterone levels drop 2% or more, per year, in aging men.
Similar to SHBG, albumin binds to testosterone in the blood and acts a carrier protein for it. It typically binds to 30-40% of circulating testosterone.
However, unlike testosterone bound to SHBG, which has a strong bond and is difficult to unbind, testosterone bound to albumin has a weaker bond and is easier to separate. This means that it is more readily available to interact with tissues and exert its physiological effects, when compared to SHBG-bound testosterone, which is significantly less bioactive.
Free testosterone refers to the portion of testosterone in the bloodstream that is not bound to any proteins. It is the active form of the male sex hormone that can directly interact with cells in the body.
Unlike testosterone bound to SHBG and albumin proteins, free testosterone isn’t attached to anything and can move freely. Of the total levels circulating the body, free testosterone makes up 1-2% of it.
The sum of free Testosterone and albumin-bound Testosterone together is referred to as Bioactive Testosterone (BT). Except from Dihydrotestosterone (DHT), these two are the most bioactive, and are therefore a primary vehicle of how the male sex hormone acts.
DHT, or dihydrotestosterone, is a hormone that is derived from testosterone. It plays an important role in male sexual development, particularly in the development of the prostate gland, external genitalia, and secondary sexual characteristics, like facial hair, body hair, and deepening of the voice.
Only a small percentage of testosterone in the body is converted into DHT (roughly 5-10%). This conversion occurs primarily in specific tissues after delivery via the bloodstream, through the action of an enzyme called 5-Alpha Reductase (5α). 5-Alpha Reductase takes testosterone and converts it into DHT.
DHT binds more strongly to androgen receptors in tissues when compared to testosterone and takes longer to wear off. This makes it between 3 – 10 times more potent! This increased potency is what allows DHT to have a greater impact on certain tissues and contribute to specific male characteristics and functions.
To increase the effects of testosterone, the more potent form of testosterone, DHT, should be maximised.
In adult males, aromatase converts a small portion of testosterone into estrogen through a process known as aromatisation. This conversion occurs primarily in adipose tissue (fat cells) and, to a lesser extent, in the testes, liver, and a few other tissues.
Approximately 0.2% of total testosterone is converted into estrogen in adult males. To maximise the levels of testosterone in the blood, this conversion should be minimised.
High levels of estrogen also inhibit the release of luteinizing hormone (the signal for leydig cells to create testosterone). As such, reducing estrogen levels not only increases the current levels of testosterone (as of the reduction in conversion), but also increases future production.
Once produced, distributed, and converted, androgens and estrogen are received by cells across the body.
Proteins named Estrogen Receptors (ERs) receive estrogen in cells, where it then has its effects. Most significantly, effecting:
Testosterone and DHT is received in cells by Androgen Receptors (ARs), where it has its effects. Most significantly, effecting:
While Testosterone Replacement Therapy (TRT) is a viable option for some men, male sex hormones can be managed to normal and healthy levels without medical treatment. Testosterone levels can be increased, and overall health can be optimised with the use of some simple techniques.
By knowing how the body works to manage testosterone levels, and what happens to it once its released, we can leverage the different mechanisms involved to increase it and the effect it has. To leverage these, we should maximise some things and minimise others.
To increase testosterone levels and maximise all the effects that come with it, maximise the following:
Increasing GnRH triggers the release of more luteinizing hormone, which in turn stimulates the leydig cells to produce more testosterone.
By increasing luteinizing hormone release, leydig cells in the testes receive more stimulation to produce testosterone.
By ensuring that leydig cells are functioning properly, we ensure that they are able to produce testosterone at a healthy rate.
By maximising DHT, the most potent androgen, you can enhance the effects of testosterone.
DHT is produced as a result of 5-alpha reductase converting testosterone to DHT. If you increase 5-alpha reductase, it will boost DHT levels, thereby enhancing the efficacy of testosterone.
By increasing androgen receptor protein expression, cells across the body are able accept and utilise testosterone and DHT more effectively, increasing the net effect they have.
To increase testosterone levels and maximise all the effects that come with it, minimise the following:
By decreasing the levels of SHBG, the amount of bound and inactive testosterone decreases. With less inactive testosterone, more is left free and active across the body, and therefore the effect it has increases.
Aromatase is responsible for converting testosterone into estrogen. If we reduce the amount of aromatase in our bodies, we reduce the amount of testosterone converted to estrogen and therefore increase circulating testosterone levels.
Estrogen also inhibits luteinizing hormone release. By reducing estrogen levels, more luteinizing hormone can be sent as a signal to leydig cells for them to produce testosterone.
Whether you have a testosterone deficiency, or just want to increase testosterone levels and the effects it has, purposefully maximising and minimising different elements can help you.
The following table summarises what should be increased and what should be decreased, and also gives some tips on how to do each.
| Element of Testosterone System | Increase/Decrease | Compounds |
|---|---|---|
| Gonadotropin Releasing Hormone (GnRH) | Increase | – |
| Luteinizing Hormone (LH) | Increase | Zinc |
| Dihydrotestosterone (DHT) and 5-Alpha Reductase | Increase | Zinc |
| Leydig Cell Function | Increase | Zinc Vitamin D |
| Androgen Receptor Protein Expression | Increase | Zinc |
| Sex Hormone Binding Globulin | Decrease | Magnesium Boron Vitamin D |
| Estrogen and Aromatase | Decrease | Boron |
Our original supplement formula for ZMAN+ contains all such compounds. Incorporate it into your daily routine and optimise your health today.


Wondering how to boost your immune defences and fight against illness? Discover the science of ZMA and how it can help your immune system.

Learn how ZMA can transform your muscle recovery and athletic performance, allowing you to reach your health goals

Studies have shown that testosterone levels are falling. Read this to find out why and what can be done to fix it.

Discover how Vitamin B6 reduces fatigue through energy metabolism, with key facts and intake recommendations.

Complete the form NOW to receive the free ebook and take on the challenge.